KAREO BILLING Eligibility Checks and Patient Authorizations
Increase Collections and Reduce Denial Rates by Verifying Patient Insurance Benefits Upfront
 Eligibility Checks and Patient Authorizations
view details
Eligibility Checks and Patient Authorizations
view details view less
view less
Kareo Billing takes the guesswork and frustrations out of checking patient insurance eligibility to help increase collections. By verifying insurance during patient registration and appointment scheduling, you can eliminate uncollectible revenue from patients due to invalid or insufficient insurance benefits. Verifying insurance coverage prior to each patient visit reduces downstream claim denials and saves the hassle caused by ineligibility.
Kareo Billing follows all industry standards for verifying insurance benefits electronically to help reduce denied insurance claims and manage patient payment responsibility. When the electronic verification is sent, an immediate response is returned with details about the patient's insurance policy, including medical services covered and the terms of the patient's copay, coinsurance, and deductible.
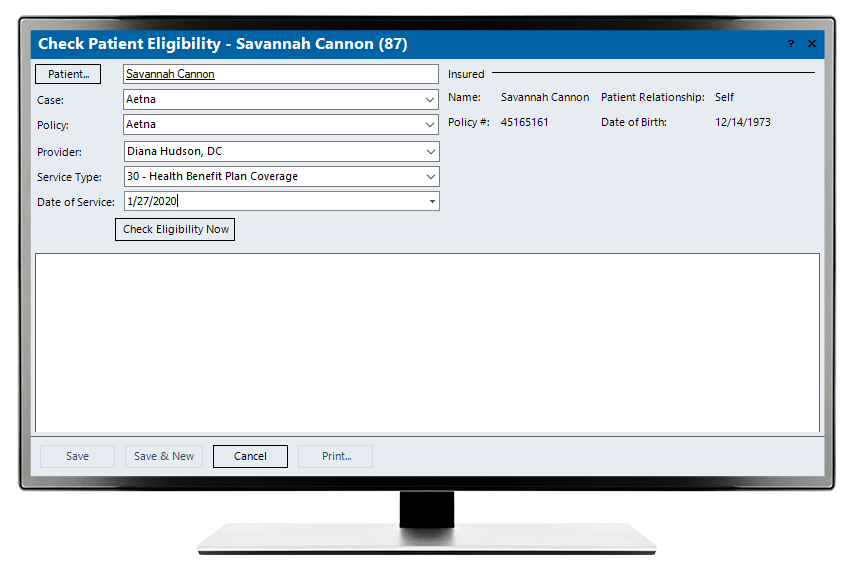
Kareo Billing assists in improving collections with an intuitive patient eligibility check.
Insurance Eligibility Delivered on the Spot
With Kareo, you can easily submit insurance eligibility inquiries to hundreds of government and commercial insurance companies including Medicare, Medicaid, Blue Cross and Blue Shield in nearly every state, and most commercial insurance companies including Aetna, Cigna, Humana, United Healthcare, and many more. All you need is basic patient information and the insurance policy data including the insurance name and policy number.
The Details You Need
Once you submit and insurance eligibility inquiry, you'll receive a response in a matter of seconds. You’ll know immediately whether the patient is covered by that insurance company. Some insurances also provide insight into the level of medical service they qualify for and the patient's payment responsibilities, such as the deductible, copayment, or coinsurance required. The insurance eligibility report can be viewed on-screen, printed, or saved to the patient's record and insurance policy file for access anytime. That’s transparency from start to finish!

Depending on insurance, billers can receive a detailed report outlining pertinent patient eligibility details for the visit.
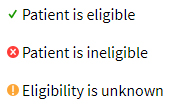
Easy to view icons show the patient’s eligibility status:
Traceable Authorizations
In Kareo Billing, users can easily access the ‘authorizations’ tab of a patient's case where information related to insurance eligibility can be added. This includes the eligibility details from the insurance company and supporting documents that provide the approval for medical services that are to be rendered to the patient. Kareo keeps track of authorized visits and automatically displays the balance of remaining authorized visits for the patient.
FEATURES
- Quick and easy electronic eligibility verification of patient insurance benefits reduces administrative burden, denials, and costs associated with verifying eligibility
- Verification and detailed eligibility available in seconds
- Save details related to eligibility directly into patient files for future reference
- Run daily batch eligibility checks prior to patient appointments that day
- Icons visually match patient eligibility status




