The Billing Manager's Guide to Avoiding MIPS Penalties
The attestation period for the MIPS 2018 Reporting Year has begun and many MIPS eligible clinicians are at risk of receiving a negative 5% payment adjustment. Don’t let that negative adjustment impact your revenue. If your clinicians are eligible for MIPS, they must submit their MIPS data before April 2nd, 2019 to avoid this payment adjustment.
Billers, You Still Have Time to Avoid MIPS Penalties
There are many reasons why eligible clinicians can fail to meet the various MIPS requirements. Perhaps a clinician switched EHRs in the middle of the year and embracing the new EHR did not come as easy as they had hoped for. Or, they are a small practice with limited resources and the provider has a complicated schedule which includes hospital rounds or patient visits in multiple medical facilities, making it difficult for them to track their performance. However, if your clinicians are subject to MIPS, they should at least submit enough points to avoid a penalty, and – let’s be honest – it is in your best interest to make sure they do!
Step 1: Check Eligibility
First, confirm your provider’s MIPS status for the MIPS 2018 Reporting Year here. You will have to enter their individual NPI. If your provider is eligible and did not meet all the requirements, you should:
- Submit at least 15 points
- Learn about the Quality Payment Program (QPP)
Step 2: Select Improvement Activities
The easiest, most cost-effective way to avoid a penalty for the 2018 Reporting Year is to submit Improvement Activities, which is worth 15% of the overall MIPS score. Therefore, if providers submit at least 15 points, they should fully meet this category.
Meet with your providers and help them select Improvement Activities from the list of 113. Improvement Activities marked ‘Medium Weighted’ are worth 10 points. Improvement Activities marked ‘High Weighted’ are worth 20 points. Make sure your providers select Improvement Activities that add up to 20-40 points to earn the full 15 points allocated to this category.
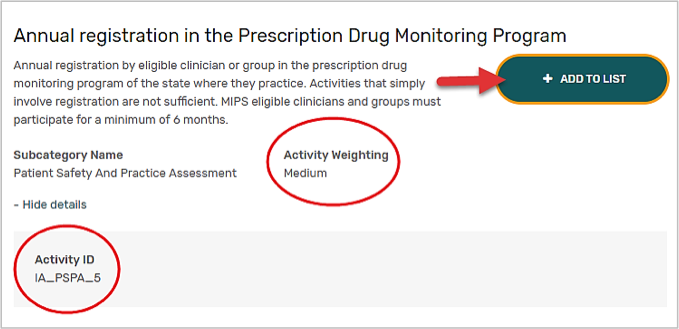
You might want to take enough time to carefully read the activity description with your providers to confirm that they have indeed completed the activity description. Then, make a note of the Improvement Activity ID and advise providers to come up with any supporting documentation that proves they completed each activity. See example below:
Step 3: Collect Supporting Documentation
Collect all supporting documentation for the selected Improvement Activities. Depending on the selection, providers may gather the following documentation:
- Screenshots: EHR and/or PM/Billing
- Create policies and procedures
- Write a statement to explain you believe you met your selected activity. Date and sign it.
- Reports
- Screenshots of a website such as a drug monitoring program
- All of the above
Providers must save the supporting documentation for a minimum of six years in case of an audit.
Step 3: Submit on the QPP Website
Finally, help the provider log in to the QPP attestation website by using their EIDM or HARP account. Once logged in, click on the link for Improvement Activities, then enter the reporting period: 90 days up to a full year. Finally, find the selected activities and click ‘Yes’ for each applicable activity. This step should take you only five minutes. Once this is done, you have successfully helped them submit enough points to avoid the MIPS negative payment adjustment.
More and more billing companies are providing MIPS reporting as an additional service to help independent medical practices comply to MACRA regulations and avoid losing out on revenue. It's a win-win for everyone.




















