We help independent practices
stay on track with MACRA
Kareo is your complete technology and business management partner for navigating the world of MACRA and getting paid in 2021.
The 21st Century Cures Act
Keeping Patients at the Center of Healthcare TechWe’re committed to providing you with key regulatory & compliance updates. Read the latest from Kareo on the 21st Century Cures Act
MACRA & MIPS Basics
MACRA is the law that governs the Medicare payment system for providers. Medicare's Quality Payment Program (QPP) is based on MACRA's rules for reimbursements and offers providers two tracks for reporting: MIPS and Advanced APMs. This guide gives an overview of what independent practices need to know.
Plan Your Path
There's no reason for any eligible clinician to pay a penalty to Medicare. Most independent practices will take the MIPS reporting track. Use the MIPS Quick-Start Checklist to see major milestones for 2021 and get started toward earning a positive payment adjustment.
Let Kareo Clinical
Certified EHR Do the Rest
See how much easier it is to report on MIPS measure with Kareo Clinical. Because Kareo's EHR is designed by doctors for doctors, there's no additional data entry for reporting on MIPS measures. You simply chart as usual, and our automated MIPS reporting and tracking system keeps you on track with earning the most in positive adjustments.
Get Higher MIPS Scores and
Earn More With Kareo
With MIPS, you can earn a positive performance-based payment adjustment on Medicare reimbursements based on your reporting score. Kareo helps you document and track progress toward your MIPS goals to make sure you earn more revenue. See how easy we make it:
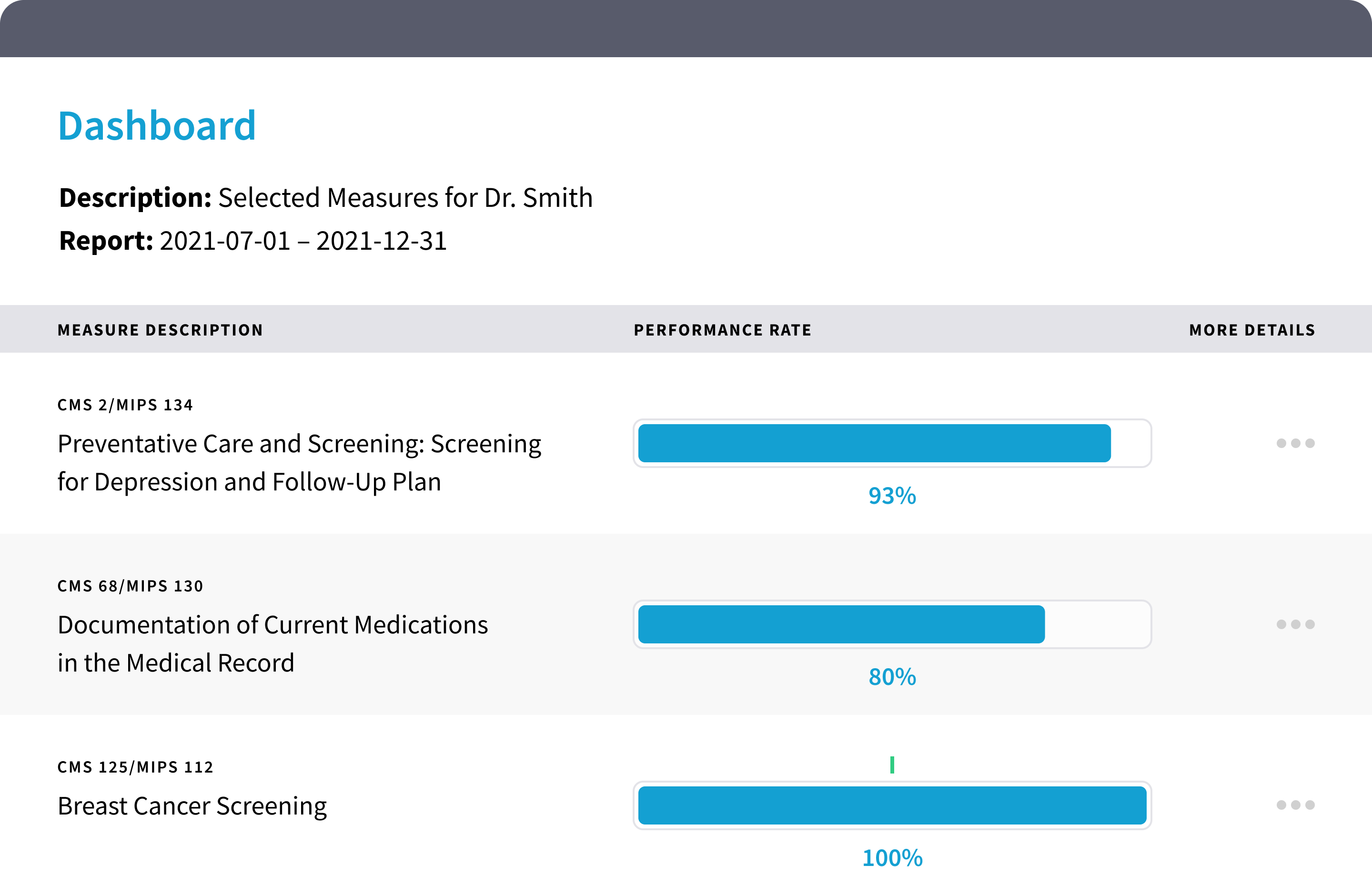
Quality Dashboard
In Kareo, it's easy to track your performance on quality measures. A simple setup wizard walks you through the steps for selecting measures. Your dashboard displays your progress and even shows you ways to improve your score.
MIPS Promoting Interoperability Dashboard
This dashboard tracks how you're doing in the Medicare Promoting Interoperability (PI) objectives and measures. The dashboard will always reflect the most current information.

Interested in learning more about how Kareo can simplify your MIPS reporting process?
Are You a Current Kareo Customer?
Learn how to take action today with step-by-step training tailored to your needs.
Frequently Asked Questions
What is MACRA?
Show
MACRA is the Medicare Access and CHIP Reauthorization Act, which is legislation that replaced the Sustainable Growth Rate (SGR). It outlines a new program for physician reimbursement that replaces fee-for-service with value-based payments under the Quality Payment Program (QPP).
What is the Quality Payment Program?
Show
The QPP is the portion of MACRA that defines the new value-based reimbursement system. It has two parts: the Merit-Based Incentive Program (MIPS) and Advanced Alternative Payment Models (APMs). The QPP replaces and consolidates the current Medicare Meaningful Use, PQRS, and value-based modifier programs.
Who participates in the QPP?
Show
The following provider types must participate in the QPP in either MIPS or APMs:
- Physician (Doctors of Medicine or Osteopathy, Doctors of Dental Surgery or Dental Medicine, Doctors of Podiatric Medicine, Doctors of Optometry, Chiropractors)
- Physician Assistant
- Nurse Practitioner
- Clinical Nurse Specialist
- Certified Registered Nurse Anesthetist
- Physical Therapist
- Occupational Therapist
- Clinical Psychologist
- Qualified speech-language pathologist
- Qualified Audiologists
- Registered dietitians or Nutrition Professionals
Do I Need a Certified EHR to participate in the Quality Payment Program?
Show
Yes, for both MIPS and the Advanced APMs, you need a certified EHR. Starting in 2018, the EHR must be 2015 Edition certified.
Are there exceptions to the eligible provider?
Show
Yes, there are two exceptions applications available to clinicians in the 2021 Performance Year:
- The Extreme and Uncontrollable Circumstances Exception.
- The MIPS Promoting Interoperability Performance Category Hardship Exception
What is the Quality requirement for MIPS?
Show
To meet the Quality requirement for MIPS for most participants, you must report up to six quality measures, including an outcome measure, for a minimum of 90 days. For those using the web interface, you must report 15 quality measures for a full year.
How many measures are there to choose from for Quality?
Show
There are 271 measures to choose from. You can select from those that best fit your practice.
What are the Improvement Activity requirements for MIPS?
Show
For most participants, the requirement for Improvement Activities for MIPS is to attest that you completed up to four improvement activities. For groups with fewer than 15 participants or if you are in a rural or health professional shortage area, the requirement is to complete up to two activities for a minimum of 90 days. If you are in a certified patient centered medical home, you automatically get full credit.
How many improvement activities are there to choose from?
Show
There are 93 improvement activities to choose from.
What is the Advancing Care Information requirement for MIPS?
Show
To meet the requirement for Advancing Care Information you need to fulfill these required measures for a minimum of 90 days:
- Security Risk Analysis
- e-Prescribing
- Provide Patient Access
- Send Summary of Care
- Request/Accept Summary of Care
You may also choose to submit up to nine measures for a minimum of 90 days for additional credit. And for bonus credit, you can also:
- Report Public Health and Clinical Data Registry Reporting measures
- Use certified EHR technology to complete certain improvement activities in the improvement activities performance category
Please note that you may not need to submit advancing care information if these measures do not apply to you.
How will we report our data for MIPS?
Show
MIPS data will be reported via the same methods as the Meaningful Use and PQRS programs. These are claims, registry, QRDC, web interface and/or CMS EHR Incentive Payment Attestation Site. During this first year, providers will most likely need to report via two methods. For example, quality measures can be reported via all methods, except the Attestation Site. Advancing Care may be reported via web interface and the Attestation Website, while the Improvement Activities will most likely be reportable via registry and Attestation Site.
Is Medicare Advantage included or does this just apply to Medicare?
Show
This program only applies to Medicare Part B.
Is it Cures Act certified?
Show
Yes, Kareo Clinical is 2015 Edition, and has implemented the 2021 Cures Act Updates. It will continue to work on the Cures Act requirements through 2022 and 2023.
Currently, I have Kareo Billing and no EHR. What are the next steps to get a certified EHR to participate in MACRA?
Show
You do need a certified EHR to participate in MACRA. You can learn more about Kareo’s EHR by calling 888-775-2736 to speak to a Kareo Solution Consultant now.
Can the required data for MIPS be captured using Kareo Clinical?
Show
Yes, Kareo Clinical provides the fields necessary to capture data for both the Quality and the Promoting Interoperability categories.Clinicians seeking to report quality measures not supported by Kareo, may still submit any measures in their specialty set when submitted via claims throughout the reporting period.The late release of the final rule does not give vendors much time to make needed updates to software. Please be patient as we do our best to get you features you need.
Will Kareo provide training on MIPS?
Show
Yes, Kareo offers live training sessions, provides recorded training webinars and training via Kareo University. Additional one-on-one support is available via our paid Professional Services

2015 Edition Cures Update Certification
This Health IT Module is 2015 Edition Cures Update compliant and has been certified by an ONC-ACB in accordance with the applicable certification criteria adopted by the Secretary of Health and Human Services. This certification does not represent an endorsement by the U.S. Department of Health and Human Services.
-
Vendor Name: Tebra Technologies, Inc.
- Website: www.kareo.com
- Address: 1111 Bayside Drive, Suite 150, Corona Del Mar, CA 92625
- Contact: Beth Lyn Onofri, Sr. Product SME - Regulatory, [email protected], (866) 93-TEBRA (83272)
- Product Version: Kareo EHR Version 5.0
- Date certified: 12/19/2022 by Drummond Group, Inc.
- Certification No: 15.04.04.2777.Kare.05.02.1.221219
- Tested and Certified Modules: 170.315(a)(1-5,9,12,14); (b)(1-3,6); (d)(1-9,12-13); (e)(1,3); (g)(2-7,9-10)
- Additional Software Required: LabSoft, Updox, DrFirst Rcopia, SmileCDR
Cost and Limitations
The monthly subscription fee for Kareo EHR v 5.0 includes all tested and certified modules listed above with exception of a one-time small set-up for implementation of e-prescribing of controlled substances. For a detailed explanation of costs and guidance, click here. Optional services, which are not required for CMS Incentive Programs, are available for a nominal fee. These services include custom template development and private CMS Incentive Programs coaching.
Real World test plans:
| Year | Test Plan | Test Result |
| 2022 | 2022 Test Plan | 2022 Test Results |
| 2023 | 2023 Test Plan |




